EEA Clinical Case Study
The Patient
An elderly woman had difficulty walking and swallowing from bony pressure on her spinal cord and brainstem due to arthritic breakdown at the top of her spine (odontoid pannus).
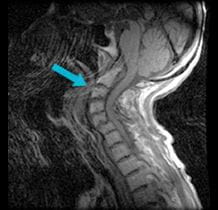
Pre-surgical scan shows bone pressing on the spinal cord and brainstem.
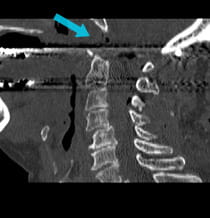
Post-surgical scan shows that bone has successfully been removed via EEA surgery to relieve pressure.
The Challenge
Traditional neurosurgical approaches to the uppermost cervical spine and its connection to the skull require an incision in the back of the throat. This keeps the patient from eating right after surgery and can potentially lead to long-term problems with swallowing. In addition, a tracheotomy is sometimes required to make room in the mouth for the traditional approach.
The Solution
Doctors at UPMC performed surgery using EEA to remove the bone that was pressing on the patient's spinal cord, rather than traditional surgery through her mouth. Because the minimally invasive surgery was performed through her nose, the patient was able to start eating the day after surgery because her mouth was not affected. As with the traditional approach, she also needed to have rods and screws placed to prevent the pressure from coming back and to stabilize the upper spine and skull.
The Result
The patient recovered very well and is walking much better now with no complication from her upper cervical spine surgery. Only her neck movement is limited from the spinal fusion, which would have been needed with any surgical approach.
Treatment and results may not be representative of all similar cases.