The Diagnosis
It was a typical doctor’s appointment for Taylor. The 20-year-old Pennsylvania Western University, Clarion, student was in her hometown of Jefferson Hills, Pa., for a routine primary care appointment in June 2021. Taylor had previously been diagnosed with anemia, so she got a blood test at her appointment. The next day, her blood work came back with a startling result.
“The results showed that I needed a blood transfusion because my hemoglobin levels were so low,” Taylor recalls. “I went to UPMC Shadyside for the blood transfusion. The doctor said he was going to run tests one more time, and when he came back in, he said that I was in stage 5 of chronic kidney disease.”
Stage 5 of chronic kidney disease (CKD) means that your kidneys are getting very close to failure or have failed. In Taylor’s case, her kidneys had failed. When your kidneys fail, dialysis or a kidney transplant become necessary.
“During that first round of dialysis, I had chest pain, was rapidly blinking, and my vision started getting fuzzy,” Taylor says. “My care team took me off the machine right away.”
Taylor’s body had gone into shock since it had been some time since she had clean blood. She says there was no way for her doctors to know how long she had been in kidney failure. A kidney biopsy showed that there were so many scars and cysts on her kidneys that no medication would reverse the disease.
“My doctors said that it was possible that I could have been born with CKD or a virus destroyed my kidneys, but there was no way to tell,” Taylor says. “I never knew I was sick. They were surprised that I wasn’t failing my classes with how horrible my lab results were. They were shocked that I was answering their questions and knew what day of the week it was.”
The speech pathology and audiology major had participated in majorettes and gymnastics since she was 5 years old. She was a captain of her college majorette team and found that her back and joints would often hurt.
“I was always tired, but I thought it was because I was a full-time college student and an athlete, and when I came home on breaks, I was working two jobs,” Taylor explains.
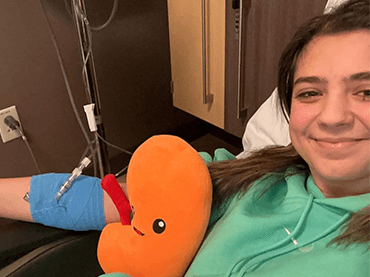
 With her new diagnosis, Taylor then began hemodialysis. Hemodialysis is a procedure where a dialysis machine and a special filter called an artificial kidney, or a dialyzer, are used to clean your blood. The machine is used for three to four hours at a time, three to four times per week, and is typically completed in a dialysis clinic.
With her new diagnosis, Taylor then began hemodialysis. Hemodialysis is a procedure where a dialysis machine and a special filter called an artificial kidney, or a dialyzer, are used to clean your blood. The machine is used for three to four hours at a time, three to four times per week, and is typically completed in a dialysis clinic.
In August 2021, Taylor was determined to still participate in band camp even though she was on hemodialysis. She would do dialysis on Mondays, Wednesdays, and Fridays at a dialysis center in North Versailles, Pa. from 7 a.m. to 10 a.m. Taylor’s mom would then drive her to Clarion, Pa. so she could attend band camp for two days, then drive her back to the dialysis center the following morning for her next session.
Eventually, Taylor was able to begin peritoneal dialysis (PD). PD does not require an artificial kidney machine to filter blood. Instead, this form of at-home dialysis uses the lining of the inside of the belly as a natural filter for blood.
“I was able to perform in all my home games that year, which was important to me,” Taylor explains. “I could feel such an improvement from my first halftime show to the last one because the dialysis was working.”
The Path to Living-Donor Kidney Transplant at UPMC
 Even though dialysis was working, Taylor still needed a kidney transplant. In June 2022, a year after her diagnosis, Taylor received a call that changed her life.
“The transplant coordinator on the phone said that they found me a living donor and asked if I wanted to schedule my transplant,” Taylor says.
Even though dialysis was working, Taylor still needed a kidney transplant. In June 2022, a year after her diagnosis, Taylor received a call that changed her life.
“The transplant coordinator on the phone said that they found me a living donor and asked if I wanted to schedule my transplant,” Taylor says.
The transplant occurred two months later on Aug. 9, 2022. Taylor’s donor was her aunt’s niece, Shelly. The next day, Taylor was able to walk. She says that her transplant was “the shortest hospital stay she had ever had.”
Taylor’s recovery went smoothly until three months later when she lost 15 pounds. She struggled to eat because her throat was swollen, and she had no appetite. Taylor was diagnosed with a rare form of lymphoma called post-transplant lymphoproliferative disorder (PTLD).
PTLD is a group of conditions that can occur after a transplant and are caused by white blood cells that multiply uncontrollably. Approximately 3% of people who have kidney transplants develop a form of PTLD. Taylor then began immunotherapy chemotherapy.
Life After Living Donation
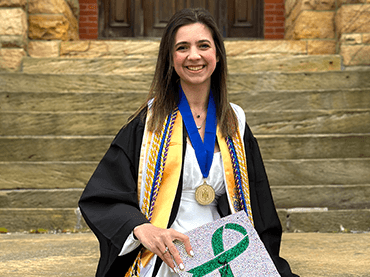
By April 2023, Taylor was in remission. She graduated college on time with high honors in May 2023 with the help of her UPMC care team and support from her family, friends, professors and her sorority, Delta Phi Epsilon.
Today, Taylor is an active advocate for the National Kidney Foundation and the American Cancer Society and speaks at events and summits. She is also continuing her education at Pennsylvania Western University, Clarion, with a master’s degree in speech language pathology.
“One of my mottos is that CKD will not define me,” Taylor says. “I told myself that I would still go to college and participate in majorettes. I want to spread as much awareness as I can because I didn’t know what kidney disease and living donation were when I was diagnosed. I also want people who are going through a chronic illness to know that you are not alone.”
Taylor and Shelly went to the Kidney Gift of Life Honors Gala together with their families and Taylor recently attended Shelly’s wedding. Shelly even has a tattoo of her and Taylor’s birth flowers, a kidney, and a green ribbon for kidney disease awareness.
“There's no real way of saying thank you for saving my life and giving me that second chance,” Taylor says. “I’m very grateful for Shelly, my family, friends, doctors, and the transplant team at UPMC. I wouldn’t be here if it wasn’t for them.”
Taylor’s treatment and results may not be representative of other cases.