The Challenge: Polycystic Kidney Disease
Ken Fitzpatrick first learned he had kidney disease at 19 years old. Doctors diagnosed him with polycystic kidney disease, where clusters of cysts form and grow in the kidneys.
“Doctors said I could probably lead a normal life, maybe never need a kidney transplant,” Ken says.
But, once he reached his 30s, he realized that living a normal life would be tough. He developed high blood pressure, leading to even more kidney damage.
Then he learned he had polycythemia, where the body makes too many red blood cells, causing the blood to get too thick.
As time went on, it was clear he would one day need a kidney transplant.
At 56 years old — after dealing with the disease his entire life — Ken’s kidney function started to decline very quickly. When his kidneys were only working at five percent, he began dialysis.
For the next year and a half, Ken went to dialysis treatments a few times a week.
Dialysis filters your blood through your body and removes waste when your kidneys are failing. Once you start treatment, you need to go a few times each week. And for people who don’t have a kidney transplant, they must be on dialysis for the rest of their lives.
So, Ken knew a transplant was vital.
The Path to Living-Kidney Donor Transplant at UPMC
After a thorough pre-transplant exam and tests, doctors approved Ken for a transplant and placed him on the kidney transplant waiting list.
Ken had less energy, missed work, and started losing hope that he would find a kidney donor. His nephew, Frank, noticed these changes and was sad to see how the dialysis treatment was affecting his uncle’s quality of life.
Ken was on the transplant waiting list for almost two years. Since over 95,000 people are on the U.S. kidney transplant waiting list, Ken knew finding a living donor was his best option.
During a living-donor kidney transplant, a surgeon removes the donor's healthy kidney and transplants it into the person with the failing kidney. The human body only needs one kidney to function, which makes this surgery possible.
To be a living-kidney donor, you must be between the ages of 18 and 69 with no history of:
- Heart disease
- Liver disease, including cirrhosis and hepatitis B and C
- Diabetes
- HIV
- Cancers or other diseases that could cause problems during surgery
Two people had evaluations to be Ken's living donor, but neither was a good match.
“That gets your hopes up,” Frank said. “Things like that kind of deflate people.”
Frank didn’t like seeing his uncle get disappointed and wanted to do something to help. He decided to get tested to be a living-kidney donor.
The Solution: Frank Gives His Uncle a New Kidney
Frank didn’t tell Ken that he made an appointment for testing to see if he could be a living donor. He wanted to keep it a secret until he knew for sure that he could donate.
He went through the extensive process to make sure he was a proper medical match for his uncle. Frank also wanted to make sure he could return to his normal life with only one kidney.
After the testing was complete, Frank happily learned he was a match and could donate. He couldn’t wait to call and tell Ken the good news.
“It was just a sigh of relief knowing that something’s going to happen,” Ken said.
In 2017, after years of struggling with kidney disease, Ken received a second chance at life thanks to his nephew’s generous gift.
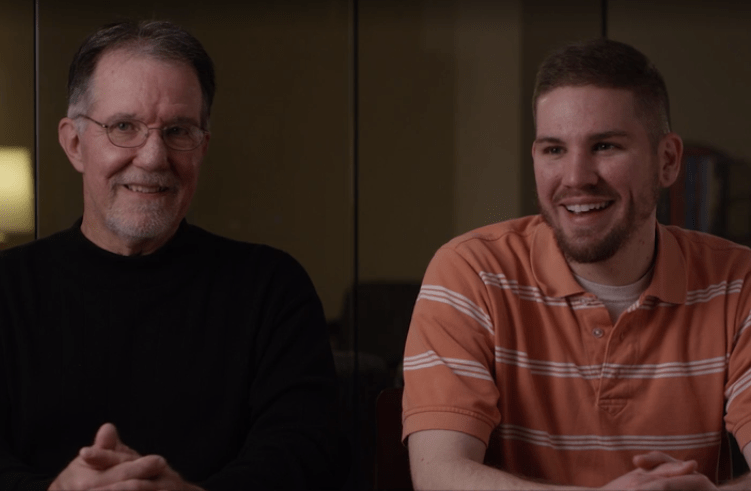
The Results: A Closer Bond Between Uncle and Nephew
After waking up in the recovery room, Ken didn’t think surgeons performed the transplant because he felt great. He was grateful that he had this chance.
“Everyone at UPMC just made everything go so smoothly,” Ken says. “I’d recommend it in a heartbeat if somebody needed a kidney.”
Today, both Ken and Frank are doing well and are even closer than they were before. Ken considers Frank a son to him, and Frank loves seeing his uncle healthy and happy again.
“I can never thank Frank more, and enough, for everything he’s done,” Ken says.
Ken and Frank’s results may not be representative of all similar cases.
Learn More About Living-Donor Kidney Transplant
From the HealthBeat blog: