What Is Endovascular Repair?
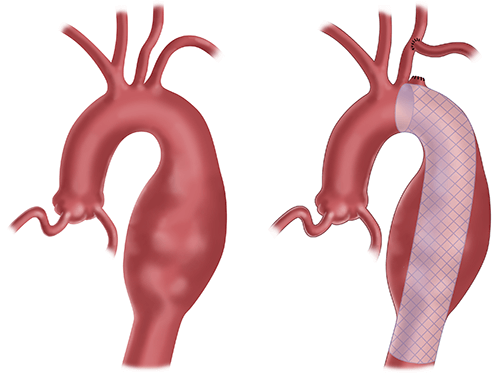
Endovascular repair is minimally invasive surgery to fix an aortic aneurysm or an aortic dissection without open surgery.
Instead of making a large incision, surgeons insert a catheter into an artery in your groin. They then place a stent into the dilated aorta to seal off the aneurysm and prevent further growth or rupture.
Your surgeon may recommend TEVAR (thoracic endovascular aortic repair) if the aneurysm is in your chest.
Contact Us
To contact the UPMC Center for Aortic Disease for more information or to make an appointment, please call 412-647-7070 or email AorticCenter@upmc.edu.
Our multidisciplinary team aims to provide timely, comprehensive, and individualized disease management strategies for patients suffering from complex thoracic aortic diseases. Learn more about our experts.
What is a TEVAR procedure?
TEVAR (thoracic endovascular aortic repair) is the stenting of an aortic aneurysm above the diaphragm.
You will receive general anesthesia for this procedure.
If your surgeon believes you are at high risk for postoperative paraplegia, you may also need a lumbar drain placed in your spinal column. The drain will help protect your spinal cord during and after TEVAR.
Neurophysiology is present for all TEVAR cases. This specialized team checks the motor responses of all extremities during the procedure. If they notice any signs of neurological problems, surgeons can intervene right away.
For thoracic endovascular aortic repairs, your surgeon will:
- Make a small cut in your groin to access an artery.
- Use an x-ray to help guide wires into the descending thoracic aorta.
- Insert stents over the wires once they’re in place and deploy the stents to repair the diseased part of the aorta.
Your surgeon may use ultrasound with contrast dye, instead of an x-ray, to guide placement and confirm results after the stent is placed.
TEVAR Risks and Benefits
All surgeries involve risk.
Complications of TEVAR may include:
- Infection.
- Bleeding.
- Blood vessel injury.
- Aortic dissection.
- Aneurysm rupture.
- Stent failure or migration during deployment.
- Kidney damage from dye used during surgery to guide stent placement.
- Paralysis of the lower body.
Recovery time is often shorter with less pain compared to open surgery.
Conditions We Treat with TEVAR
Our surgeons at UPMC are experts in treating thoracic aortic aneurysms and aortic dissections.
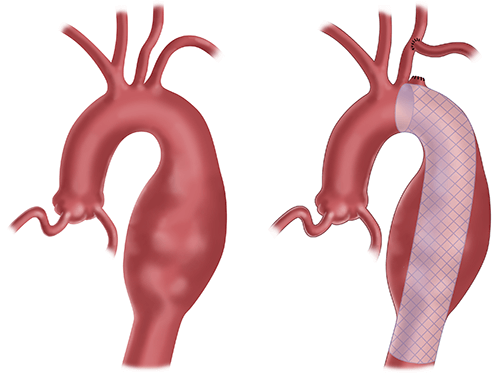
A descending thoracic aortic aneurysm is a bulging, weakened area in the wall of the aorta, in the section that runs downward through the chest.
Regardless of your diagnosis, you'll receive the highest quality of care from the UPMC Center for Aortic Disease. We work closely with other UPMC experts to offer a complete team approach to treatment.
How to Prep for Your TEVAR Surgery
Your surgeon will plan your aortic aneurysm or dissection treatment based on your:
- Precise diagnosis
- Anatomy
- Other health problems
Treatment may involve either:
- Watchful waiting (serial CT scans and blood pressure control with drugs).
- Or surgery with TEVAR, or open thoracoabdominal aortic repair.
If you and your surgeon agree that endovascular repair is the best way to treat your aortic aneurysm, you'll need to prepare.
You'll need pre-op testing including:
- CT scans
- Blood tests.
- Urine tests.
- Chest x-rays.
- Echocardiogram of your heart.
- EKG.
- Lung function tests if you smoke or have a history of lung disease.
- Doppler ultrasound of your carotid arteries.
Your surgeon will let you know if or when you need to stop taking any medications before surgery.
What to Expect Before, During, and After TEVAR
Before TEVAR
On the day of your surgery, before going into the OR:
- A nurse will place an IV in your arm and may draw blood.
- An anesthesiologist and a member of the surgical team will examine you. They'll answer last-minute questions and help you sign consent forms.
- If our team determines that you need a lumbar drain, a member of the care team will place a small catheter in your back to drain fluid from around your spinal cord. This helps improve blood flow to the spinal cord after surgeons place the stent and decreases the chances of leg paralysis.
During TEVAR
The anesthesia team will put you to sleep using general anesthesia. They will then place a breathing tube down your throat and place you on a ventilator. This machine will breathe for you during surgery.
A nurse will insert a catheter in your bladder.
During TEVAR your surgeon will:
- Make a small cut in your groin and place a sheath in your femoral artery.
- Advance a wire through the sheath into the aorta and thread a stent over the wire.
- Use ultrasound, radiograph, and IV dye to locate exactly where the stents should go.
- Place one or more stents to seal off the aneurysm and prevent further growth or rupture.
After TEVAR
Once your surgeon finishes your operation:
How long will I be in the hospital after TEVAR?
If you had TEVAR, your total hospital stay will last about a week. During your stay, you'll work with cardiac rehab and physical therapy on walking.
TEVAR Recovery
After your endovascular repair surgery:
- You'll need to take it easy at home for 4 to 6 weeks.
- A home nurse will visit you 2 or 3 times per week for 2 to 4 weeks. These visits will include vital signs, exams, medication monitoring, and blood draws.
- You may also need home occupational or physical therapy.
How you may feel during recovery
As you heal from TEVAR you may have:
- Groin pain where your surgeon made the incision.
- Shortness of breath.
- Fatigue or lack of energy.
- Swelling in the arms, hands, legs, or feet.
- Trouble sleeping.
- Short-term mood changes, including anxiety or depression.
Post-op restrictions
It's vital to follow your surgeon's instructions during recovery.
That means:
- No driving until after your 4 week follow-up visit with your surgeon. It's fine to ride in a car in the meantime.
- Don't lift anything heavier than 10 pounds.
- Lift your legs above your heart whenever you sit.
- Take brief walks each day to regain your strength.
- Blow into your incentive spirometer at least 10 times per hour. Using this device fills your lungs with air and helps prevent post-op issues like pneumonia.
Follow-up Tests and Appointments After Endovascular Repair Surgery
You will have your follow-up visit 4 to 6 weeks after leaving the hospital.
You may need to have some tests done before that visit, such as:
- CT angiogram
- Echocardiogram
- EKG
If your test results are normal, you can resume driving after this visit. You can also return to work and most other normal activities.
Expect to have your next appointment between 6 and 12 months.
You'll also need to schedule visits with your heart doctor and PCP.